Pain and perception – exploring the mind-body connection in treating chronic pain
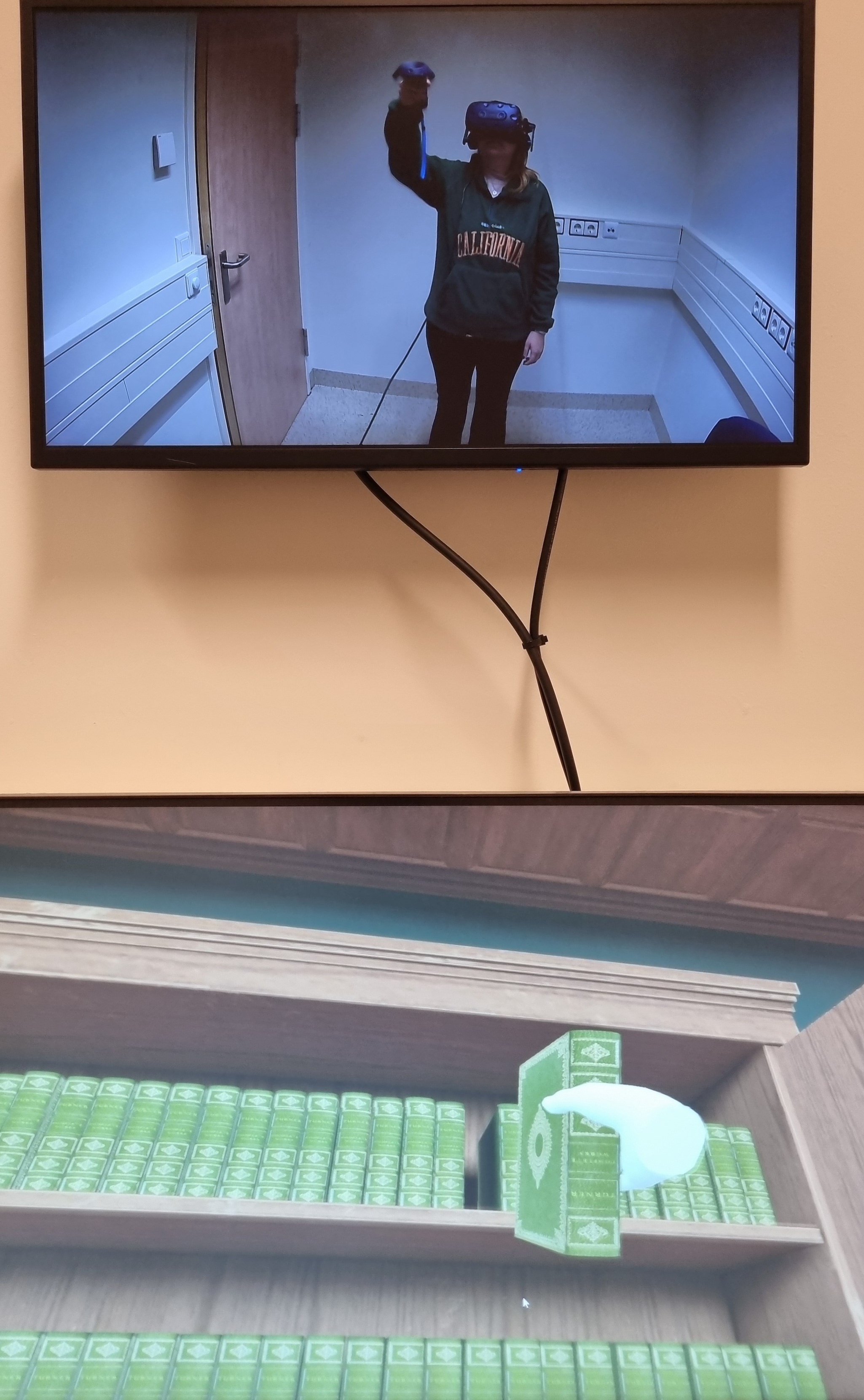
In a small room at Maastricht University in the Netherlands, a woman wearing a virtual reality headset is busy stacking virtual books onto a virtual bookcase. Every time she bends down, electrodes deliver a sharp zap of electricity to her lower back under the watchful eyes of a researcher tracking her performance, reactions and eye movements.
The unusual scene is part of a study being led by Dr Dimitri Van Ryckeghem, Assistant Professor of experimental health psychology at the University of Maastricht. The researcher's aim is to unravel the complex relationship between attention processes, avoidance behaviour and pain in an effort to determine how and why pain becomes chronic.
Attention bias
Back in 2016, the University of Luxembourg received funding from the EU to explore how the relationship between mind and body can affect chronic pain.
“In the long term, increased attention to uncontrollable pain may result in more negative pain outcomes.
In the initial two-year study, called PainDynamics and coordinated by the University of Luxembourg, Van Ryckeghem and colleagues looked at the issue of attention bias, a natural tendency to focus on negative or pain-related information.
While this had already been studied in a laboratory setting, they moved their research into the real world. This let them dispel a number of assumptions which can help refine new therapeutic approaches.
For a long time, researchers thought that people experiencing chronic pain pay too much attention to pain-related information, such as potential pain triggers, making the pain worse and turning it into a chronic vicious circle.
While this is true, it doesn’t mean that paying attention to pain is fundamentally a bad thing, as was long believed. Van Ryckeghem and his colleagues argued that this attention bias is the brain’s way of trying to keep us safe, by alerting us to potential danger.
Breaking the pain cycle
Unfortunately, this protective instinct can also be detrimental. Focusing on pain that cannot be addressed in the moment, at the expense of other important goals, can magnify it and make acute pain chronic over time.
“In the long term, increased attention to uncontrollable pain may result in more negative pain outcomes. This may be something we could target,” said Van Ryckeghem, who is hoping his work will help develop effective psychological interventions that could help break the pain cycle.
However, his 2016 research showed that attention bias changes with a person’s goals, and simply training people to pay less attention to pain without taking that into account does not help to reduce pain, as was previously believed.
Building on this breakthrough, the research team are now digging even deeper, investigating the impact that our memories and interpretations have on pain and avoidant behaviour.
“All these cognitive processes are related to each other,” said Van Ryckeghem. “The more you interpret ambiguous situations as negative, the more you will be attentive to them.”
Lost in interpretation
There is a tendency in people with chronic pain to interpret all pain as part of the same problem, such as assuming that sore muscles are connected to chronic pain, even when this might not be the case.
This is known as an interpretation bias. The researchers believe that modifying the way a person interprets physical signals or underlying variables could be a promising avenue for treatment.
According to the European Pain Federation, chronic pain affects an estimated 150 million people across Europe (about one in five adults) and can have a devastating impact on quality of life.
There is also a heavy social and economic cost to pay as a result of people being unable to work or having to rely heavily on already stretched healthcare systems. New strategies are needed for dealing with pain and making it more manageable.
Reasons for chronic pain are extremely varied and it can affect people in different ways. These include chronic back pain, arthritis, neuropathic pain caused by injury or trauma, as a result of cancer or diabetes, or chronic health conditions where the underlying cause of the pain is unclear.
Vicious circle
One unfortunate demonstration of the close relationship between mind and body is the connection between chronic pain and mood disorders. According to a 2022 review in Translational Psychiatry, up to 61% of chronic pain patients suffer from depression, while as many as 65% of depressed people also experience chronic pain. Sufferers of chronic pain can become trapped in a vicious circle.
Take someone with chronic back pain, for example, said Dr Ipek Yalcin, head of the Pain and Psychopathology research team at the Institute of Cellular and Integrative Neuroscience (INCI) in Strasbourg, France.
“They have less social interaction because they cannot go out as much, they cannot do sports, which reinforces the risk of psychiatric disorders.”
Pain erodes key cornerstones of wellbeing, such as exercise, sleep and socialising. In the case of long-term chronic pain, this can lead to depression and anxiety.
“It’s so obvious, but we don’t understand the underlying mechanisms,” said Yalcin.
Further complicating the matter is the fact that people with mood disorders are also more likely to develop chronic pain.
“Sometimes it’s very complicated to know which comes first, the chicken or the egg,” she said.
Mental and physical
Despite that, few researchers have the necessary background in studying both pain and depression. That is why Yalcin set up HaPpY, an EU-funded multidisciplinary European Joint Doctorate programme for young researchers, which launched in 2021 and will conclude in the summer of 2025.
The researchers are supported in their work by a network of universities and research institutes, as well as clinical centres and industry partners.
“The aim was to gather researchers from the fields of pain and psychiatry to better understand the underlying mechanisms of this comorbidity and find new treatment strategies,” said Yalcin.
“Drugs developed based on male data might not work for the whole population.
Comorbidity is the simultaneous presence of two or more medical conditions in a patient.
Ginevra Sperandio, one of the 14 young researchers in the programme, has found the exchange with colleagues from other disciplines invaluable.
“Having the opportunity to engage with people from different fields and ask fundamental questions has been incredibly beneficial,” the Italian researcher said.
Attention bias has also come up in her own research on post-surgical pain in breast cancer patients, which shows that certain thought patterns correlate with chronic pain after surgery.
“Catastrophising, overwhelming worries and rumination can contribute to chronic pain, probably because of the mental fixation on it,” she said.
The gender pain gap
The researchers are working to understand better the relationship between pain and mood disorders and the mechanisms that fuel it. They are also developing new treatment strategies, taking into account another often-overlooked factor in pain: gender.
By now, the gender pain gap is well-documented, but rarely addressed. While women are more likely to experience chronic pain, they are less likely to be believed and will often wait longer for a diagnosis, claim researchers.
Despite that, clinical studies often disregard the impact of gender, said Yalcin. This is why researching the impact of gender differences is a fundamental objective of HaPpY.
“We see more and more that the underlying mechanisms are different. This means that drugs developed based on male data might not work for the whole population,” said Yalcin, who is optimistic about closing the gender pain gap.
“I think awareness is starting to increase at all levels, and we are on the right track.”
Research in this article was funded by the Marie Skłodowska-Curie Actions (MSCA). The views of the interviewees don’t necessarily reflect those of the European Commission. If you liked this article, please consider sharing it on social media.




