 StatCan COVID-19: Data to Insights for a Better CanadaImpacts of the COVID-19 pandemic in nursing and residential care facilities in Canada
StatCan COVID-19: Data to Insights for a Better CanadaImpacts of the COVID-19 pandemic in nursing and residential care facilities in Canada
Introduction
In the last 10 years, there has been very little information collected nationally on residential care facilities despite about 500,000 Canadians living in these settings (Statistics Canada, 2016). Significant data gaps exist concerning these facilities and their residents, which has been further highlighted by the COVID-19 pandemic.
Of the 500,000 Canadians living in residential care facilities, the vast majority (425,000) live in either nursing homes (also known as long-term care homes) or seniors’ homes (also known as retirement homes or assisted living facilities) (Statistics Canada, 2016). These facilities in particular have been among the hardest hit by the COVID-19 pandemic in Canada. During the first wave of the pandemic (March through August 2020), residents of nursing and seniors’ homes accounted for more than 80% of all reported COVID-19 deaths (Canadian Institute for Health Information, 2020). Furthermore, infections among staff at these facilities represented more than 10% of the country’s total cases (9,500 cases, including 9 deaths) (Canadian Institute for Health Information, 2020). By mid-December (partway through the second wave that lasted from September 2020 through February 2021), there were about 44,000 cases and 9,200 deaths in nursing and seniors’ homes (Public Health Agency of Canada, 2020). As of early March 2021, reports indicated that nursing and seniors’ homes continued to account for the greatest proportion of outbreak-related cases and deaths, representing about 7% of all cases and more than 50% of all deaths (Public Health Agency of Canada, 2021a, 2021b). Many residents of nursing and seniors’ homes are at increased risk for negative outcomes of the virus (such as hospitalization or death) as they are older and more likely to have complex chronic conditions (Industry Canada, 2020). Residential care facilities in general are potentially at higher risk for the spread of infection given the unavoidable close contact between staff and residents (Industry Canada, 2020).
This article presents preliminary results on the impact of the COVID-19 pandemic in nursing homes and seniors’ homes as well as mental health facilities and other residential care facilities (such as group homes for persons with disabilities or addictions, homes for women, etc.) in Canada during the period up to and including December 31, 2020. Results presented are from 4,217 of the 5,260 residential care facilities that respondedNote 1 to the recently completed 2020 Nursing and Residential Care Facility Survey.
Nearly all facilities reported implementing new or increased Infection Prevention and Control procedures in response to the pandemic
Regular hand washing and environmental cleaning and disinfection are among the many daily practices recommended for preventing the spread of infection in settings such as residential care facilities. With the emergence of the COVID-19 pandemic, public health authorities recommended additional infection prevention and control (IPC) measures such as the regular use of personal protective equipment (PPE) such as masks, gloves or gowns (Government of Canada, 2020). Results of the survey suggest that nearly all responding facilities implemented one or more new or increased IPC measures in response to the pandemic (data not shown). About 9 out of 10 facilities also introduced other public-health recommended changes, such as the reconfiguration of furniture, the regular testing for COVID-19 among residents and staff or the increased use of virtual care services. Some of the most commonly reported changes are presented in Chart 1, by facility type.

Data table for Chart 1
| New or increased protocol | Type of facility | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Nursing homes | Seniors' homes | Mental health facilities | Other care facilities | |||||||||
| % | from | to | % | from | to | % | from | to | % | from | to | |
| Re-configuration of furniture | 82.6 | 80.2 | 84.8 | 73.6 | 71.6 | 75.5 | 53.9 | 48.3 | 59.5 | 43.6 | 40.4 | 46.8 |
| Introduction or increased use of virtual care services | 65.0 | 62.0 | 67.8 | 35.5 | 33.4 | 37.7 | 49.7 | 44.1 | 55.3 | 44.0 | 40.8 | 47.3 |
| COVID-19 testing of residents | 82.5 | 80.1 | 84.7 | 65.5 | 63.4 | 67.6 | 46.4 | 40.8 | 52.0 | 44.4 | 41.1 | 47.6 |
| COVID-19 testing of staff | 82.2 | 79.7 | 84.4 | 73.0 | 71.0 | 74.9 | 45.4 | 39.9 | 51.0 | 45.6 | 42.4 | 48.8 |
| Screening of residents/visitors/employees | 96.2 | 94.8 | 97.2 | 89.1 | 87.7 | 90.4 | 89.1 | 85.1 | 92.2 | 91.6 | 89.6 | 93.2 |
| Personal protective equipment practices | 97.3 | 96.2 | 98.1 | 97.0 | 96.2 | 97.7 | 95.1 | 92.0 | 97.0 | 96.1 | 94.7 | 97.2 |
| Hand hygiene | 94.6 | 93.0 | 95.8 | 94.3 | 93.2 | 95.3 | 96.4 | 93.6 | 98.0 | 96.1 | 94.7 | 97.2 |
|
Note: At this time, these results are considered preliminary and are subject to change. Results refer to protocols newly introduced or increased at any point up to and including December 31, 2020. Source: Nursing and Residential Care Facility Survey 2020. |
||||||||||||
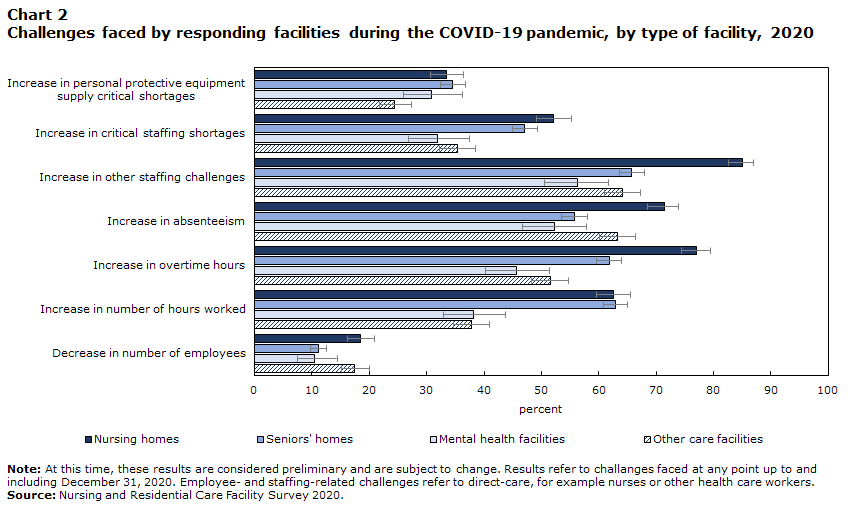
Nursing homes were more likely to experience staffing-related challenges
Despite all of the public-health measures taken by facilities, many facilities still reported facing many important challenges at some point in 2020 as a result of the pandemic (Chart 2). For example, about 86% of facilities reported experiencing at least one staffing-related challenge in 2020 (data not shown); however, nursing homes were much more affected by certain staffing challenges compared to other types of facilities (Chart 2).
Data table for Chart 2
| Challenges faced | Type of facility | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Nursing homes | Seniors' homes | Mental health facilities | Other care facilities | |||||||||
| % | from | to | % | from | to | % | from | to | % | from | to | |
| Increase in personal protective equipment supply critical shortages | 33.5 | 30.7 | 36.4 | 34.5 | 32.5 | 36.7 | 30.9 | 26.0 | 36.3 | 24.4 | 21.7 | 27.3 |
| Increase in critical staffing shortages | 52.2 | 49.2 | 55.2 | 47.1 | 44.9 | 49.3 | 31.9 | 26.9 | 37.4 | 35.4 | 32.3 | 38.5 |
| Increase in other staffing challenges | 85.0 | 82.7 | 87.0 | 65.8 | 63.7 | 67.9 | 56.3 | 50.6 | 61.7 | 64.2 | 61.0 | 67.3 |
| Increase in absenteeism | 71.4 | 68.5 | 74.0 | 55.8 | 53.6 | 58.0 | 52.3 | 46.7 | 57.9 | 63.3 | 60.1 | 66.4 |
| Increase in overtime hours | 77.1 | 74.4 | 79.5 | 61.8 | 59.6 | 63.9 | 45.7 | 40.2 | 51.4 | 51.6 | 48.3 | 54.8 |
| Increase in number of hours worked | 62.6 | 59.7 | 65.5 | 62.9 | 60.8 | 65.1 | 38.2 | 32.9 | 43.7 | 37.8 | 34.7 | 41.0 |
| Decrease in number of employees | 18.5 | 16.2 | 20.9 | 11.1 | 9.8 | 12.6 | 10.5 | 7.5 | 14.5 | 17.4 | 15.1 | 20.0 |
|
Note: At this time, these results are considered preliminary and are subject to change. Results refer to challanges faced at any point up to and including December 31, 2020. Employee- and staffing-related challenges refer to direct-care, for example nurses or other health care workers. Source: Nursing and Residential Care Facility Survey 2020. |
||||||||||||
Among nursing homes, 77% reported an increase in the number of overtime hours, 71% reported an increase in absenteeism and 85% reported other staffing challenges among direct-care employees such as nurses or other health care workers (Chart 2). More than half of nursing homes also reported critical staffing shortages, which was defined as a shortage of staff, particularly in key roles (such as directors of care, nurses or personal support workers) that had an impact on the quality of resident care and employee safety. Furthermore, about one-third of nursing homes reported experiencing critical shortages in PPE in 2020. Some studies have indicated that health care workers may be at increased risk of mental health impacts due to increased risk of exposure and demanding working conditions. A recent crowdsource survey of health care workers in Canada reported that 70% of health care workers indicated their mental health was somewhat or much worse now compared to before the pandemic, and more than half (56%) reported that most days were quite a bit or extremely stressful (Statistics Canada, 2021).
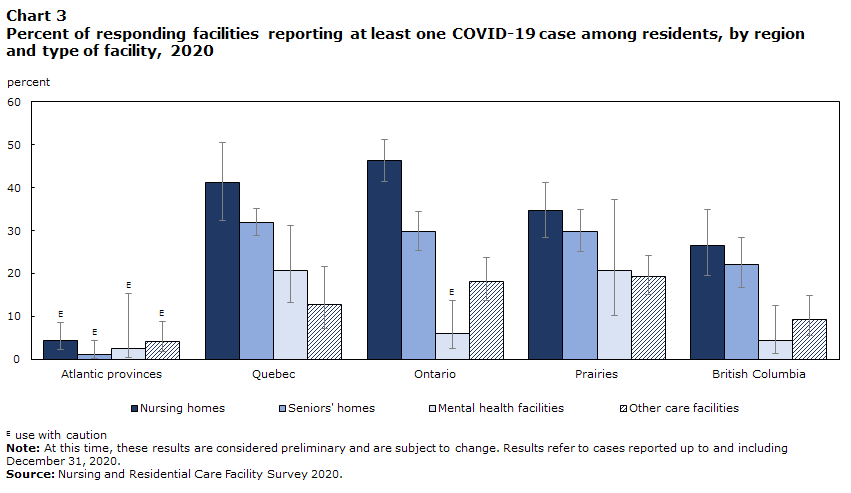
Nursing homes and seniors’ homes were more likely to report at least one COVID-19 case among residents compared to other types of facilities
Chart 3 shows that the percent of responding residential care facilities that reported a COVID-19 outbreak (defined as at least one case among residents (Canadian Institute for Health Information, 2020)) at any point in 2020 was highest in Ontario (32% of facilities), followed by QuebecNote 2 (31% of facilities), the Prairies (27% of facilities), British Columbia (17% of facilities), and the Atlantic provinces (3% of facilities) (data not shown). Outbreaks were generally higher in nursing homes and seniors’ homes compared to other facilities, though the differences were not always statistically significant (Chart 3).
Data table for Chart 3
| Region | Type of facility | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Nursing homes | Seniors' homes | Mental health facilities | Other care facilities | |||||||||
| % | from | to | % | from | to | % | from | to | % | from | to | |
| Atlantic provinces | 4.4Note E: Use with caution | 2.2 | 8.5 | 1.1Note E: Use with caution | 0.3 | 4.3 | 2.4Note E: Use with caution | 0.3 | 15.4 | 4.1Note E: Use with caution | 1.9 | 8.9 |
| Quebec | 41.1 | 32.4 | 50.4 | 31.9 | 28.9 | 35.1 | 20.8 | 13.1 | 31.3 | 12.8 | 7.2 | 21.6 |
| Ontario | 46.3 | 41.5 | 51.1 | 29.8 | 25.5 | 34.5 | 6.0Note E: Use with caution | 2.5 | 13.7 | 18.2 | 13.7 | 23.8 |
| Prairies | 34.6 | 28.5 | 41.3 | 29.7 | 25.1 | 34.9 | 20.6 | 10.1 | 37.3 | 19.2 | 15.1 | 24.2 |
| British Columbia | 26.6 | 19.6 | 34.9 | 22.0 | 16.7 | 28.4 | 4.4 | 1.4 | 12.6 | 9.2 | 5.5 | 15.0 |
|
E use with caution Note: At this time, these results are considered preliminary and are subject to change. Results refer to cases reported up to and including December 31, 2020. Source: Nursing and Residential Care Facility Survey 2020. |
||||||||||||
The impact of COVID-19 in nursing and seniors’ homes has been widely covered in the media and several reports and inquiries have taken place in an effort to reduce the risk of infection, outbreaks and associated deaths in the future (Canadian Institute for Health Information, 2021b; Government of Nova Scotia, 2020; Ontario Long-Term Care Commission, 2021; Office of the Auditor General of Ontario, 2021; Revera, 2020). As was the case for these reports, an important goal of the recent NRCFS was to contribute to the better understanding of the factors associated with increased rates of COVID-19 infection.
Logistic regression analysis of a subset of facilitiesNote 3 suggests that among responding nursing homes, facilities were at greater risk of an outbreak if they reported: having at least one case among employees, being a larger facility (more than 50 residents), and having experienced an increase in critical staffing shortages (Table 1). Among responding seniors’ homes, facilities were at greater risk for an outbreak if they reported: at least one case among employees and being a larger facility (more than 25 residents). COVID-19 cases among staff was the most significant predictor of outbreaks: facilities that reported at least one case among employees were about 4 times more likely to have experienced an outbreak, and among seniors’ homes, those facilities were nearly 7 times more likely. For seniors’ homes, having only private rooms at the facility was also associated with a decreased risk of outbreaks.
| Characteristic | Nursing homes | Seniors' homes | ||||
|---|---|---|---|---|---|---|
| Adjusted risk ratioTable 1 Note 1 | 95% Confidence interval | Adjusted risk ratioTable 1 Note 1 | 95% Confidence interval | |||
| from | to | from | to | |||
| For profit status | ||||||
| For profit | 1.04 | 0.90 | 1.20 | 1.11 | 0.96 | 1.27 |
| Not for profitTable 1 Note † | Note ...: not applicable | Note ...: not applicable | Note ...: not applicable | Note ...: not applicable | Note ...: not applicable | Note ...: not applicable |
| Types of rooms | ||||||
| Private rooms only | 0.94 | 0.79 | 1.11 | 0.86Note * | 0.76 | 0.97 |
| Shared roomsTable 1 Note † | Note ...: not applicable | Note ...: not applicable | Note ...: not applicable | Note ...: not applicable | Note ...: not applicable | Note ...: not applicable |
| Size of facility (number of residents) | ||||||
| 25 or fewer residentsTable 1 Note † | Note ...: not applicable | Note ...: not applicable | Note ...: not applicable | Note ...: not applicable | Note ...: not applicable | Note ...: not applicable |
| 26 to 50 residents | 1.80 | 0.92 | 3.51 | 1.56Note * | 1.22 | 2.00 |
| 51 to 100 residents | 2.48Note * | 1.31 | 4.66 | 1.67Note * | 1.29 | 2.16 |
| 101 or more residents | 3.52Note * | 1.87 | 6.63 | 2.17Note * | 1.69 | 2.79 |
| Registered nurses on staff | ||||||
| Yes | 0.85 | 0.68 | 1.07 | 0.93 | 0.82 | 1.06 |
| NoTable 1 Note † | Note ...: not applicable | Note ...: not applicable | Note ...: not applicable | Note ...: not applicable | Note ...: not applicable | Note ...: not applicable |
| At least one employee case reported | ||||||
| Yes | 4.16Note * | 2.91 | 5.93 | 6.57Note * | 5.26 | 8.22 |
| NoTable 1 Note † | Note ...: not applicable | Note ...: not applicable | Note ...: not applicable | Note ...: not applicable | Note ...: not applicable | Note ...: not applicable |
| Critical staffing shortagesTable 1 Note 2 | ||||||
| Increased | 1.22Note * | 1.04 | 1.43 | 1.08 | 0.96 | 1.22 |
| Decreased or no changeTable 1 Note † | Note ...: not applicable | Note ...: not applicable | Note ...: not applicable | Note ...: not applicable | Note ...: not applicable | Note ...: not applicable |
| Personal protective equipment shortagesTable 1 Note 3 | ||||||
| Increased | 1.02 | 0.87 | 1.20 | 1.00 | 0.88 | 1.14 |
| Decreased or no changeTable 1 Note † | Note ...: not applicable | Note ...: not applicable | Note ...: not applicable | Note ...: not applicable | Note ...: not applicable | Note ...: not applicable |
... not applicable
Source: Nursing and Residential Care Facility Survey 2020. |
||||||
These results are in line with previously published research in Canada which have shown that larger facilities (National Collaborating Centre for Methods And Tools 2020; Canadian Institute for Health Information 2021b), facilities having shared rooms (Brown et al. 2020), and facilities reporting cases among employees (Fisman et al. 2020) were more likely to have experienced outbreaks or to have more severe outbreaks.
Other research has shown many other factors to be associated with outbreaks in nursing or seniors’ homes such as a lack of availability of registered nurses (National Collaborating Centre for Methods And Tools 2020) or personal support workers (Canadian Institute for Health Information 2021b). However, these factors were not significant when included in the present analysis. For-profit status has also been suggested to be associated with outbreaks during this pandemic (NCCMT 2020; Stall et al. 2020). For-profit status was not found to be significant in the present analysis either, which is similar to more recent findings in an Ontario report which found that for-profit status was not significantly associated with either the severity of outbreaks or the resident mortality rate after controlling for other factors (Canadian Institute for Health Information 2021b).
Other factors that have been shown or suggested to be significantly related to COVID-19 cases or deaths in nursing and seniors’ homes include: being part of a large chain of facilities (Canadian Institute for Health Information 2021b), having a smaller ratio of nursing staff to residents (Canadian Institute for Health Information 2021b), having a greater proportion of older residents (National Collaborating Centre for Methods And Tools 2020), having a greater proportion of male residents (National Collaborating Centre for Methods And Tools 2020), as well as the number of cases in the surrounding community (National Collaborating Centre for Methods And Tools 2020; Canadian Institute for Health Information 2021b). These factors were not considered in the current analysis due to a lack of availability or the need for additional data review and validation, but may be evaluated in future analyses.
Conclusion
Preliminary data from the 2020 Nursing and Residential Care Facility Survey show that, among responding facilities, the majority of responding residential care facilities in Canada reported, at some point up to and including December 31, 2020, making changes to IPC practices, such as introducing or increasing practices such as hand washing and use of PPE or making other changes to the facility such as the installation of partitions or the regular testing of residents or staff. However, the majority of responding facilities also reported facing important challenges such as an increase in absenteeism among staff. Several responding facilities even reported significant staffing shortages or shortages in PPE supplies during this reference period. The preliminary data also suggest that after controlling for region, among responding facilities, large facilities, cases among employees and staffing shortages were associated with an outbreak in nursing homes, while shared rooms, large facilities and cases among employees were associated with outbreaks in seniors’ homes. However, more research is needed to better understand the impact of the pandemic on nursing and residential care facilities in Canada.
Data source & methods
Data for this analysis are from the 2020 Nursing and Residential Care Facility Survey (NRCFS), a national survey targeting public and private sector establishments classified to code 623 “Nursing and residential care facilities” of the North American Industry Classification System (NAICS) 2017. This includes nursing homes, seniors’ homes, mental health facilities and other care facilities (such as homes for women, or substance use facilities). Data were collected directly from respondents using an electronic questionnaire. Collection took place from January 5 to March 31, 2021. At the time of analysis, the overall response rate for the survey was 66% (n = 5,260 facilities). Response rates were generally higher in the private sector (71%) than in the public sector (55%)Note 2 and varied by province (as high as 79% in Nova Scotia and as low as 54% in Newfoundland and Labrador). The overall response rate in the territories was less than 25%. Included in this article are responding facilities that reported having at least one bed, at least one resident and at least one employee (n = 4,217). Excluded were those that did not meet the listed criteria, had missing or invalid data, or were considered to be out of scope for the survey.
The survey collected basic information on facility characteristics, such as employee and resident counts for the 2019/2020 fiscal year, as well as information related to the COVID-19 pandemic up to and including December 31, 2020. Basic descriptive statistics are used to describe the many changes and challenges faced by each type of facility during the pandemic. In nursing and seniors’ homes, logistic regression was used to assess the relationship between certain facility characteristics (including: region, for-profit status, private or shared rooms, number of residents, registered nurses on staff, cases among employees, critical staffing shortages and personal protective equipment shortages) and the risk of an outbreak, defined as one or more COVID-19 cases among residents. Results are presented as risk ratios, which compares the risk of an outbreak for one group (e.g. Ontario) versus another group (e.g. Quebec), adjusted for all other listed variables. A risk ratio greater than 1 indicates an increased risk and a risk ratio less than 1 indicates a decreased risk.
References
Brown KA, Jones A, Daneman N, et al. 2021. “Association between nursing home crowding and COVID-19 infection and mortality in Ontario, Canada” JAMA Internal Medicine, 181(2):229-236
Canadian Institute for Health Information. 2020. Pandemic Experience in the Long-Term Care Sector: How Does Canada Compare with Other Countries? Ottawa, ON: CIHI.
Canadian Institute for Health Information. 2021a. The Impact of COVID-19 on Long-Term Care in Canada: Focus on the First 6 Months. Ottawa, ON.
Canadian Institute for Health Information. 2021b. “Factors associated with COVID-19 outbreaks, transmission and poor outcomes in Ontario’s LTC homes: Presentation to the Ontario Long-Term Care Commission”.
Fisman DN, Bogoch I, Lapointe-Shaw L, McCready J, and Tuite AR. 2020. “Risk factors associated with mortality among residents with coronavirus disease 2019 (COVID-19) in long-term care facilities in Ontario, Canada” JAMA Network Open, 3(7):e2015957
Government of Canada. 2021. “Infection prevention and control for COVID-19: Interim guidance for long-term care homes”.
Government of Nova Scotia. 2020. COVID-19 First Wave Review: March to September 2020. Halifax, NS.
Industry Canada. 2020. “Long-Term Care and COVID-19: Report of a Special Task Force Prepared for the Chief Science Advisor of Canada”.
National Collaborating Centre for Methods and Tools. 2020. “What risk factors are associated with COVID-19 outbreaks and mortality in long-term care facilities and what strategies mitigate risk?”
Office of the Auditor General of Ontario. 2021. COVID-19 Preparedness and Management: Special Report on Pandemic Readiness and Response in Long-Term Care. Toronto, ON.
Public Health Agency of Canada. 2020. “Canada COVID-19 Weekly Epidemiological Report (13 December to 19 December, 2020)”
Public Health Agency of Canada. 2021a. “COVID-19 daily epidemiological update”.
Public Health Agency of Canada. 2021b. “Canada COVID-19 Weekly Epidemiological Report: 28 February to 06 March 2021 (Week 09)”
Revera. 2020. Revera Pandemic Report: A Perfect Storm – The COVID-19 Experience for Revera and the Long-Term Sector.
Stall NM, Jones A, Brown KA, Rochon PA and Costa AP. 2020. “For profit long-term care homes and the risk of COVID-19 outbreaks and resident deaths” CMAJ, 192(33):E946-E955
Statistics Canada. 2016. “Type of Collective Dwelling (16) and Collective Dwellings Occupied by Usual Residents and Population in Collective Dwellings (2) of Canada, Provinces and Territories, 2016 Census - 100% Data”, Statistics Canada Data Table no. 98-400-X2016019
Statistics Canada. 2021. “Mental health among health care workers in Canada during the COVID-19 pandemic”.
- Date modified: