Abstract
Objective
We examined the safety and efficacy of endoscopic stone removal for choledocholithiasis in elderly patients ≥90 years of age with native papilla and compared the outcomes with those in patients 75-89 years of age.
Methods
This multicenter retrospective study included 569 patients 75-89 years of age and 126 patients ≥90 years of age who had native papilla and underwent therapeutic endoscopic retrograde cholangiopancreatography (ERCP) for choledocholithiasis at 3 institutions in Japan between April 2012 and March 2018. The main outcomes assessed were the incidence of post-ERCP complications during hospitalization and outcomes of ERCP in patients ≥90 years of age.
Results
Biliary cannulation and subsequent endoscopic sphincterotomy, endoscopic balloon dilation, and endoscopic large balloon dilation were successful in 97.7% of patients 75-89 years of age and in 98.4% of patients ≥90 years of age. There was no significant difference in the incidence of post-ERCP complications between patients 75-89 years of age and those ≥90 years of age (7.7% vs. 9.5%, respectively; p=0.47). Although the rate of use of mechanical lithotripter was not significantly different, the rate of complete stone removal in patients ≥90 years of age was lower than that in patients 75-89 years of age (81.0% vs. 94.9%, respectively; p<0.001). In all cases with incomplete stone removal in both groups, permanent biliary stent placement was successful.
Conclusion
ERCP for choledocholithiasis in elderly patients ≥90 years of age is a safe and effective procedure; however, endoscopists should select appropriate strategies after considering each patient's medical condition and background.
Keywords: ERCP, common bile duct stone, elderly patient, oldest-old
Introduction
According to the 2017 World Population Prospects report by the United Nations, the global increase in life expectancy is contributing to a progressive increase in the proportion of the elderly population (1). Approximately 5% of all patients with cholecystitis have co-existing common bile duct (CBD) stones; among elderly patients with cholecystitis, this percentage is as high as 10-20% (2). Owing to the higher prevalence of CBD stones in the elderly population, endoscopic stone removal in elderly patients is likely to increase in the future.
Although endoscopic removal of CBD stones using endoscopic retrograde cholangiopancreatography (ERCP) is an effective procedure, it is associated with a high risk of post-ERCP complications, such as post-ERCP pancreatitis (PEP), cholangitis, bleeding, and perforation, in addition to common endoscopic complications, such as pneumonia (3), which pose serious problems for elderly patients.
In Japan, an age of ≥75 years is classified as old age, while individuals ≥90 years of age are classified as oldest-old (4). Previous studies have investigated the efficacy and safety of therapeutic ERCP for elderly patients using a cut-off age of 80-85 years (5-8); there have been only a few studies on the efficacy and safety of endoscopic stone removal in elderly patients ≥90 years of age. Previous studies published in 2000 and 2006 showed that there was no significant difference in the incidence of post-ERCP complications between elderly patients ≥90 years of age and elderly patients 70-89 years of age. In elderly patients ≥90 years of age, the rate of complete stone removal was lower, additional ERCP attempts were required to achieve stone clearance, and mechanical lithotripters were used more frequently than in those 70-89 years of age (9,10).
However, these studies included small populations of elderly patients ≥90 years of age, and endoscopic papillary large balloon dilation (EPLBD) has become increasingly popular following the publication of these reports. We therefore examined the efficacy and safety of endoscopic stone removal in a large cohort of elderly patients ≥90 years of age and compared their outcomes with those observed in elderly patients 75-89.
Materials and Methods
Patient selection and study design
Medical records pertaining to patients who had undergone therapeutic ERCP for choledocholithiasis at three institutions in Japan between 2012 and March 2018 were retrospectively reviewed. The inclusion criteria were as follows: (1) elderly patients ≥75 years of age with choledocholithiasis; (2) patients with native papilla who underwent endoscopic sphincterotomy (EST), endoscopic papillary balloon dilation (EPBD), or EPLBD; and (3) patients with a normal gastrointestinal tract or Billroth I reconstruction. The exclusion criteria were as follows: (1) patients ≤74 years of age; (2) history of EST, EPBD, or EPLBD; and (3) history of Billroth II or Roux-en-Y reconstruction. A total of 695 elderly patients ≥75 years of age (569 elderly patients 75-89 years of age and 126 elderly patients ≥90 years of age) met the study selection criteria and were included in this study (Figure).
Figure.
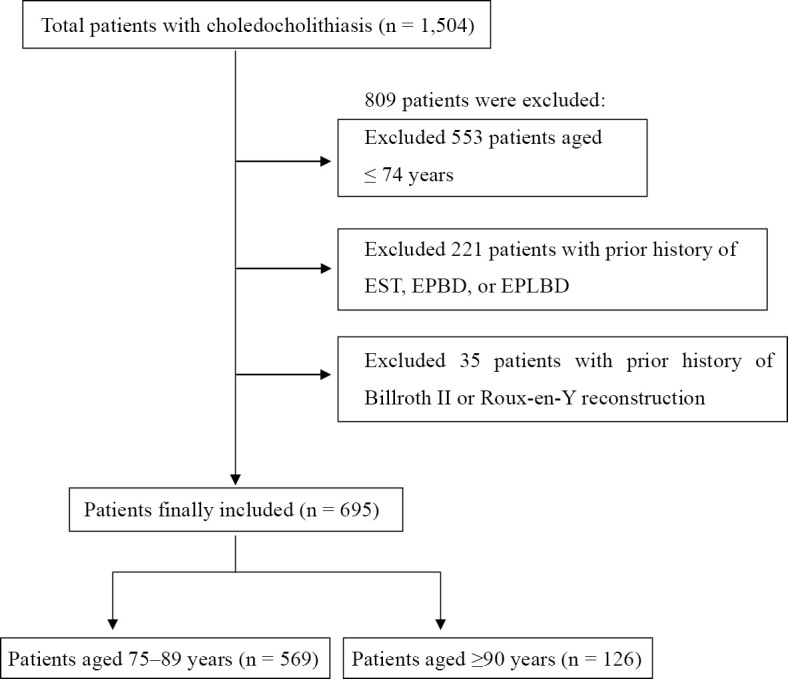
Flowchart of enrolled patients. EST: endoscopic sphincterotomy, EPBD: endoscopic papillary balloon dilation, EPLBD: endoscopic papillary large balloon dilation
This study was approved by the Institutional Review Boards of each of the participating institutions. Informed consent was obtained from all patients prior to their enrollment.
Outcomes
The primary outcome of this study was the incidence of post-ERCP complications during hospitalization. Secondary outcomes were the frequency of mechanical lithotripter use, the number of successful procedures (complete stone removal or permanent biliary stent placement), and the number of ERCP sessions associated with a successful procedure.
Study definitions
•Trainee endoscopists
Trainee endoscopists were defined as endoscopists who had performed <200 ERCP procedures or who could perform only procedures equivalent to Grade 1 with or without assistance, according to the ERCP core curriculum published in 2016 (11).
•Post-ERCP complications
Post-ERCP complications were defined as all complications that occurred after the ERCP procedure and during hospitalization. Post-ERCP complications included PEP, bleeding, perforation, acute cholangitis/cholecystitis, pneumonia, and cardiovascular and cerebrovascular events. Acute cholangitis/cholecystitis was diagnosed and graded based on the Tokyo guidelines 2018 (12). Post-ERCP complications, except for acute cholangitis/cholecystitis, were diagnosed and graded based on a lexicon for endoscopic adverse events (13).
•Incomplete stone removal and successful procedure
Incomplete stone removal was defined as cases with successful cannulation wherein complete stone removal could not be achieved (excluding cases with unsuccessful cannulation). A successful procedure was defined as complete stone removal or permanent biliary stent placement in cases with incomplete stone removal.
•Emergency ERCP
Emergency ERCP was defined as ERCP performed within 24 hours of the choledocholithiasis diagnosis.
•Severe medical conditions as the reason for incomplete clearance
Severe medical conditions were defined as the reason for incomplete clearance in cases with an unstable cardio-respiratory condition before ERCP or with a high risk of deterioration of the cardio-respiratory condition during or after ERCP.
Diagnostic procedure
One or more imaging examinations, including computed tomography (CT), magnetic resonance cholangiopancreatography (MRCP), endoscopic ultrasonography (EUS), ultrasonography (US), and cholangiography via percutaneous transhepatic gallbladder drainage tube (PTGBD), were performed for the diagnosis of CBD stones in all patients. In cases not diagnosed by imaging examinations, clinical findings such as abdominal pain, dilated CBD, and/or elevated liver function tests were used to establish the diagnosis. The Tokyo guidelines 2018 were used for the diagnosis and grading of acute cholangitis (12).
Criteria for performing ERCP for choledocholithiasis at our institutions
At our institutions, the criteria for ERCP for choledocholithiasis required patient consent for the procedure, including detailed information regarding post-ERCP complications. Patients could not exhibit respiratory or circulatory dysfunction if they were to undergo ERCP.
Therapeutic procedure
Twenty-five endoscopists were included in this study. Nine of these 25 were trainee endoscopists. ERCP procedures performed by trainee endoscopists were assisted by experienced endoscopists. Side-viewing duodenoscopes (Olympus JF-260, TJF-260V; Olympus Medical Systems, Tokyo, Japan) were used in all patients. Intravenous midazolam and/or pethidine hydrochloride were administered for sedation. The doses of midazolam and pethidine hydrochloride were determined based on the sedation protocol at our institutions.
In patients 75-89 years of age who weighed <70 kg, the doses of midazolam and pethidine hydrochloride were 1 mg and 17.5-35 mg, respectively, while the doses in those who weighed ≥70 kg were 2 mg and 17.5-35 mg, respectively. In patients ≥90 years of age, the doses of midazolam and pethidine hydrochloride were 1 mg and 17.5 mg, respectively, regardless of weight. Scopolamine butylbromide or glucagon was used for duodenal relaxation. After biliary cannulation, EST, EPBD, or EPLBD followed by biliary stent placement or stone removal was performed. EPLBD was indicated for patients with large and/or multiple stones, with CBD dilation, which were difficult to remove by either EST or EPBD. One or more devices, including balloon catheter, basket, and/or a mechanical lithotripter, were used to remove the CBD stones. A permanent biliary stent was placed in patients with a poor performance status, severe medical condition, and multiple and/or large stones that were difficult to remove based on the endoscopist's decision.
Statistical analyses
Between-group differences with respect to the demographic and clinical characteristics, ERCP-related findings and outcomes, the reasons for incomplete stone removal, and complications and severity of ERCP were assessed using the chi-squared test, Fisher's exact test, or t-test, as appropriate. All statistical analyses were performed using R version 3.5.1 (http://www.R-project.org). P values <0.05 were considered indicative of statistically significant differences.
Results
Demographic and clinical characteristics
Demographic and clinical characteristics of the study population are presented in Table 1. Compared to patients 75-89 years of age, significantly more elderly patients ≥90 years of age underwent emergency ERCP, had severe acute cholangitis, exhibited a dilated common bile duct (>10 mm), and had a poor performance status (3 or 4). Although not statistically significant, patients ≥90 years of age were more likely to exhibit large stones (>10 mm) and multiple large stones, compared with patients 75-89 years of age.
Table 1.
Demographic and Other Characteristics of the Study Population.
| Patients aged 75-89 years (n=569) | Patients aged ≥90 years (n=126) | ||||
|---|---|---|---|---|---|
| n | % | n | % | p value | |
| Age range (years) | 75-89 | 90-104 | |||
| Sex (female) | 284 | 49.9 | 87 | 69.0 | <0.001 |
| Emergency ERCP | 400 | 70.3 | 108 | 85.7 | <0.001 |
| Clinical presentation | |||||
| Acute cholangitis | |||||
| Mild cholangitis | 147 | 25.8 | 32 | 25.4 | 1.0 |
| Moderate cholangitis | 165 | 29.0 | 46 | 36.5 | 0.12 |
| Severe cholangitis | 42 | 7.4 | 19 | 15.1 | 0.010 |
| Biliary pancreatitis | 54 | 9.5 | 19 | 15.1 | 0.091 |
| Obstructive jaundice without cholangitis | 35 | 6.2 | 2 | 1.6 | 0.065 |
| Elevated liver test with normal serum bilirubin and without cholangitis | 48 | 8.4 | 4 | 3.2 | 0.065 |
| asymptomatic CBD stones | 78 | 13.7 | 4 | 3.2 | 0.002 |
| Chronic concomitant diseases | |||||
| Hemodialysis | 12 | 2.1 | 0 | 0 | 0.14 |
| Cardiovascular disease | 101 | 17.8 | 24 | 19.0 | 0.83 |
| Cerebrovascular disease | 57 | 10.0 | 14 | 11.1 | 0.84 |
| Liver cirrhosis | 6 | 1.1 | 1 | 0.8 | 1.0 |
| Diabetes mellitus | 65 | 11.4 | 9 | 7.1 | 0.21 |
| ≥2 comorbidities | 74 | 13.0 | 13 | 10.3 | 0.50 |
| Antithrombotic drugs | 197 | 34.6 | 33 | 26.2 | 0.086 |
| Peri-ampullary diverticulum | 175 | 30.8 | 46 | 36.5 | 0.25 |
| Diameter of common bile duct [mean, (range)], mm | 11.7 (4-30) | 13.1(5-25) | <0.001 | ||
| Dilated common bile duct (>10 mm) | 334 | 58.7 | 92 | 73.0 | 0.004 |
| Number of stones [mean, (range)] | 2.3 (0-20) | 2.1 (0-15) | 0.57 | ||
| Multiple stones | 228 | 40.1 | 53 | 42.1 | 0.75 |
| Size of stones [mean, (range)], mm | 7.9 (2-25) | 9.4 (3-30) | 0.077 | ||
| Large stone (>10 mm) | 115 | 20.2 | 36 | 28.6 | 0.052 |
| Multiple and large stones | 67 | 11.8 | 23 | 18.3 | 0.070 |
| Gallbladder stones | 332 | 58.3 | 73 | 57.9 | 1.0 |
| Post-cholecystectomy | 62 | 10.9 | 15 | 11.9 | 0.87 |
| Performance status (3 or 4) | 124 | 21.8 | 55 | 43.7 | <0.001 |
ERCP: endoscopic retrograde cholangiopancreatography, CBD: common bile duct
Diagnostic modality for CBD stones
The imaging modalities used for the diagnosis of CBD stones were MRCP [79/695 (11.4%)], CT [466/695 (67.1%)], US [28/695 (4.0%)], EUS [2/695 (0.3%)], and PTGBD [2/695 (0.3%)]. More than 2 modalities were used in 118 (17.0%) patients. CBD stones were detected in 574 of the 695 (82.6%) patients by at least 1 imaging modality; in the remaining 121 patients, a clinical diagnosis of CBD was made. In 628 of the 680 (92.4%) patients who underwent successful cannulation, CBD stones were actually detected during ERCP.
Findings and outcomes of ERCP
ERCP-related findings and outcomes are presented in Table 2. No significant differences were observed between elderly patients 75-89 years of age and elderly patients ≥90 years of age with respect to the proportions of procedures performed by trainee endoscopists, the rate of successful cannulation, pancreatic guidewire-assisted cannulation, pancreatic injections, precut sphincterotomy, EST, EPBD, EPLBD, cannulation time >10 minutes, prophylactic pancreatic stent placement, or procedure time. Complete stone removal was achieved in 540 of the 569 (94.9%) elderly patients 75-89 years of age and in 102 of the 126 (81.0%) elderly patients ≥90 years of age (p<0.001). In both groups, a permanent biliary stent was successfully placed in all patients with successful cannulation where complete stone removal could not be achieved. No significant between-group differences were observed regarding the use of a mechanical lithotripter, mean number of ERCP sessions per patient required for a successful procedure, and the mean hospital stay duration.
Table 2.
ERCP-related Findings and Outcomes in Patients Aged 75-89 and ≥90 Years.
| Patients aged 75-89 years (n=569) | Patients aged ≥90 years (n=126) | ||||
|---|---|---|---|---|---|
| n | % | n | % | p value | |
| Successful cannulation | 556 | 97.7 | 124 | 98.4 | 1.0 |
| •Complete stone removal | 540 | 94.9 | 102 | 81.0 | <0.001 |
| •Incomplete stone removal | 16 | 2.8 | 22 | 17.5 | <0.001 |
| Unsuccessful cannulation | 13 | 2.3 | 2 | 1.6 | 1.0 |
| Trainee endoscopist | 98 | 17.2 | 21 | 16.7 | 0.98 |
| PGW-assist cannulation | 113 | 19.9 | 29 | 23.0 | 0.50 |
| Pancreatic injections | 286 | 50.3 | 66 | 52.4 | 0.74 |
| Precut sphincterotomy | 31 | 5.4 | 6 | 4.8 | 0.93 |
| EST | 382 | 67.1 | 84 | 66.7 | 1.0 |
| EPBD | 76 | 13.4 | 16 | 12.7 | 0.96 |
| EPLBD | 98 | 17.2 | 24 | 19.0 | 0.72 |
| Cannulation time>10 min | 171 | 30.1 | 37 | 29.4 | 0.96 |
| Mechanical lithotripter | 113 | 19.9 | 26 | 20.6 | 0.94 |
| Permanent biliary stent placement | 16 | 2.8 | 22 | 17.5 | <0.001 |
| Prophylactic pancreatic stent | 98 | 17.2 | 25 | 19.8 | 0.57 |
| Procedure time (SD), min | 27.6 (15.1) | 29.8 (20.0) | 0.16 | ||
| ERCP attempts for successful procedure [mean (range)] | 2.0 (1-7) | 1.9 (1-6) | 0.13 | ||
| Hospital stay (mean), days | 13.1 | 14.7 | 0.081 | ||
ERCP: endoscopic retrograde cholangiopancreatography, PGW: pancreatic guide-wire, EST: endoscopic sphincterotomy, EPBD: endoscopic papillary balloon dilation, EPLBD: endoscopic papillary large balloon dilation
Reasons for incomplete stone removal
The reasons for incomplete stone removal are presented in Table 3. Among patients with incomplete stone removal, significantly more patients ≥90 years of age were unable to tolerate complete stone removal because of severe medical conditions or a poor performance status or dementia than patients 75-89 years of age.
Table 3.
The Reasons for Incomplete Stone Removal in Patients Aged 75-89 and ≥90 Years.
| Patients aged 75-89 years (n=556) | Patients aged ≥90 years (n=124) | ||||
|---|---|---|---|---|---|
| n | % | n | % | p value | |
| Severe medical conditions intolerable for stone removal | 1 | 0.2 | 6 | 4.8 | <0.001 |
| Poor performance status or dementia | 12 | 2.2 | 14 | 11.3 | <0.001 |
| Multiple and large stones | 3 | 0.5 | 2 | 1.6 | 0.23 |
Incidence of post-ERCP complications
Of the 695 patients, 56 (8.1%) experienced post-ERCP complications during hospitalization, including PEP, cholangitis/cholecystitis, bleeding, perforation, pneumonia, and cardiovascular and cerebrovascular events. The incidence of complications among patients 75-89 years of age and patients ≥90 years of age was 7.7% (44/569) and 9.5% (12/126), respectively. There were no significant differences in the incidences of post-ERCP complications between patients 75-89 years of age and patients ≥90 years of age (Table 4).
Table 4.
Incidence of Complications Related to ERCP in Patients Aged 75-89 and ≥90 Years.
| Patients aged 75-89 years (n=569) | Patients aged ≥90 years (n=126) | ||||
|---|---|---|---|---|---|
| n | % | n | % | p value | |
| Post-ERCP pancreatitis | 21 | 3.7 | 2 | 1.6 | 0.41 |
| Acute cholangitis/cholecystitis | 11 | 1.9 | 2 | 1.6 | 1.0 |
| Bleeding | 4 | 0.7 | 3 | 2.4 | 0.12 |
| Perforation | 2 | 0.4 | 0 | 0 | 1.0 |
| Pneumonia | 3 | 0.5 | 3 | 2.4 | 0.076 |
| Heart failure | 1 | 0.2 | 1 | 0.8 | 0.33 |
| Complete atrioventricular block | 1 | 0.2 | 0 | 0 | 1.0 |
| Cerebral infarction | 0 | 0 | 1 | 0.8 | 0.18 |
| Respiratory dysfunction | 1 | 0.2 | 0 | 0 | 1.0 |
ERCP: endoscopic retrograde cholangiopancreatography
Severity of post-ERCP complications and mortality
The severity of post-ERCP complications and mortality rates are shown in Table 5. There were no significant between-group differences with respect to the severity of post-ERCP complications. The overall mortality rate in our study population was 0.14% (1/695).
Table 5.
Severity of Post-ERCP Complications in Patients Aged 75-89 and ≥90 Years.
| Patients aged 75-89 years (n=44) | Patients aged ≥90 years (n=12) | ||||
|---|---|---|---|---|---|
| n | % | n | % | p value | |
| Mild | 23 | 52.3 | 5 | 41.7 | 0.74 |
| Moderate to severe | 20 | 45.5 | 7 | 58.3 | 0.64 |
| Death | 1 | 2.3 | 0 | 0 | 1.0 |
ERCP: endoscopic retrograde cholangiopancreatography
Discussion
In the present retrospective study, we compared the safety and efficacy of endoscopic stone removal between elderly patients ≥90 years of age and elderly patients 75-89 years of age. No significant between-group differences were observed with respect to the incidence of post-ERCP complications. Although there was no significant between-group difference with respect to the rate of use of mechanical lithotripter, the rate of complete stone removal in elderly patients ≥90 years of age was significantly lower than that in elderly patients 75-89 years of age.
Several studies have assessed the safety and efficacy of endoscopic removal of CBD stones in elderly patients using the cut-off age of 80-85 years. The results showed that the safety and efficacy of endoscopic stone removal in elderly patients is comparable to that in younger patients (5-8). In Japan, patients ≥90 years of age are defined as the oldest-old patients (4), and a few studies with small sample sizes have assessed the efficacy and safety of stone removal using ERCP in this population. For example, a study found no significant difference in the incidence of post-ERCP complications between elderly patients ≥90 years of age (n=22) and those 70-89 years of age (n=381) [5% (1/22) vs. 7% (26/381), respectively]. However, the rate of duct clearance was lower in elderly patients ≥90 years of age than in those 70-89 years of age (86% vs. 95%, respectively) (9). Another study that included 63 patients ≥90 years of age with pancreatobiliary diseases (including 51 with CBD stones) found no significant difference in the rate of post-ERCP complications between patients ≥90 years of age and those 70-89 years of age [6.3% (4/63) vs. 8.3% (29/350), respectively]. However, the number of ERCP attempts for stone clearance was higher, and the use of mechanical lithotripter was more frequent among patients ≥90 years of age than in those 70-89 years of age (10).
In the present study, there was no significant difference in the incidence of post-ERCP complications between patients 75-89 years of age and those ≥90 years of age (7.7% and 9.5%, respectively), and the incidence of moderate-to-severe complications was also comparable between the groups (45.5% and 58.3%, respectively). The reasons for the comparable incidence of post-ERCP complications and complication severity in the two patient groups might be patient selection and the selection of appropriate endoscopic strategies. At our institutions, patients who met the criteria for ERCP for choledocholithiasis underwent ERCP. Severe cholangitis was more frequently observed in patients ≥90 years of age than in those 75-89 years of age. Patients who were unable to tolerate ERCP were treated by alternative methods, such as antibiotics and percutaneous biliary drainage. Alternative methods were therefore more frequently used in patients ≥90 years of age than in those 75-89 years of age in the present study. Furthermore, permanent stent placement was performed in high-risk patients with a poor performance status or dementia, severe medical conditions, or large and/or multiple stones that were difficult to remove, based on the endoscopist's decision. Therefore, when performing ERCP, especially in elderly patients ≥90 years of age, appropriate patient selection and appropriate selection of endoscopic strategies is important.
Although a previous report showed that use of a mechanical lithotripter was more frequent in patients ≥90 years of age (9,10), no significant between-group difference was observed in the present study. This might be because patients ≥90 years of age with large and/or multiple stones were treated with EPLBD in our study. EPLBD, first reported in 2003, is effective for removing multiple and large CBD stones that are difficult to remove using EPBD or EST alone (14). In previous studies, stone clearance rates for large stones (>12-15 mm) without the use of the mechanical lithotripter were 89-99% in patients treated with EPLBD (14-16). In the present study, EPLBD was performed in patients with multiple and/or large stones. Patients ≥90 years of age were more likely than those 75-89 years of age to exhibit multiple and/or large stones, although this difference was not statistically significant. This may explain the lack of any significant between-group differences in the frequency of mechanical lithotripter use in the present study.
In the present study, elderly patients ≥90 years of age had a more severe medical condition, poorer performance status, and larger stones than those 75-89 years of age; therefore, the rate of stone clearance was significantly lower than in patients 75-89 years of age (81.0% vs. 94.9%, respectively). These findings are in agreement with earlier reports (9). A previous report showed that biliary stent placement for two months resulted in partial or complete resolution of large or multiple stones without any complications (17). For patients in whom complete stone removal is difficult to achieve due to large or multiple stones, regardless of the use of mechanical lithotripter or EPLBD, biliary stent placement at the initial ERCP and subsequent stone removal after two months may be an effective strategy. Long-term biliary stent placement is another alternative strategy for elderly patients with unsuccessful stone clearance. In a prospective study, the patency rates of plastic biliary stent for choledocholithiasis at 6, 12, and 24 months were 94%, 79%, and 58%, respectively (18). In a systematic review, the mean incidence rates of late complications, biliary-related mortality, and non-biliary-related mortality were 23%, 3.3%, and 20.5%, respectively (19). Long-term biliary stent placement and close follow-up to detect late complications, such as stent obstruction, are viable options for elderly patients with a poor performance status, severe medical conditions, and multiple and/or large stones.
Appropriate sedation is essential for the success of ERCP procedures. However, sedation can cause oxygen desaturation and/or hypotension. Airway obstruction and respiratory depression have been shown to be the most critical risk factors for mortality associated with endoscopic procedures performed under sedation. The incidence rates outside the operating room were two times higher than inside the operating room (20). In the present study, there were no significant between-group differences in cardio-respiratory complications, possibly because the dose of medication for sedation was determined by the patient's age and weight, based on our institutions' protocols. However, one of our patients discontinued ERCP after EST because of oxygen desaturation caused by sedation. Fortunately, this patient underwent complete stone removal a few days later. ERCP should be carried out under careful vital sign monitoring, especially in elderly patients.
Although the incidence of post-ERCP complications in patients ≥90 years of age was comparable with that in patients 75-89 years of age in this study, a previous study that examined the risk factors for complications of ERCP among patients ≥85 years of age found that only age ≥90 years was a significant risk factor for therapeutic ERCP (21). Another study showed that elderly patients ≥75 years of age tended to experience more severe complications during endoscopic stone removal than patients <75 years of age (22). Therefore, detailed counseling of elderly patients and their caregivers about the risks of post-ERCP complications is imperative prior to performing ERCP.
Several limitations associated with the present study warrant mention. First, the present study was a retrospective study. Second, one of the participating institutions suffered extensive damage during the Kumamoto earthquake in April 2016. Owing to the disruption caused by the earthquake, the data obtained from that institution pertained only to a 4-year period (April 2012 to April 2016). Third, only patients who met the criteria for ERCP for choledocholithiasis at our institutions were analyzed. We did not determine the proportion of elderly patients 75-89 years of age and ≥90 years of age who were treated by alternative methods (without ERCP), such as antibiotics and percutaneous biliary drainage. Furthermore, permanent stent placement was performed in patients with a poor performance status or dementia, severe medical conditions, or large and/or multiple stones that were difficult to remove, based on the endoscopist's decision. Therefore, because our study population was defined by our institutions' criteria and our endoscopists' decisions, a selection bias likely exists. Fourth, the long-term outcomes of ERCP in elderly patients ≥90 years of age are unclear because the primary outcome of this study was post-ERCP complications during hospitalization.
In conclusion, we found that the incidence of post-ERCP complications during hospitalization in elderly patients ≥90 years of age was similar to that in elderly patients 75-89 years of age. Although the complete stone removal rate was lower in elderly patients ≥90 years of age than in those 75-89 years of age, biliary stent placement was successful in all patients with incomplete stone removal. Among elderly patients with choledocholithiasis ≥90 years of age, ERCP is a safe and effective procedure; however, when performing ERCP in very elderly patients, endoscopists should consider the risks of ERCP based on each patient's medical condition and background and select the appropriate strategy for the patients.
The authors state that they have no Conflict of Interest (COI).
Acknowledgement
We thank the staff involved in therapeutic ERCP for choledocholithiasis at the participating institutions.
References
- 1.United Nations, Department of Economic and Social Affairs, Population Division (2017). World Population Prospects: The 2017 Revision, Key Findings and Advance Tables. ESA/P/WP/248 [Internet]. [cited 2017 Jun. 16]. Available from: https://population.un.org/wpp/Publications/Files/WPP2017_KeyFindings.pdf
- 2. Siegel JH, Kasmin FE. Biliary tract diseases in the elderly: management and outcomes. Gut 41: 433-435, 1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Anderson MA, Fisher L, Jain R, et al. Complications of ERCP. Gastrointest Endosc 75: 467-473, 2012. [DOI] [PubMed] [Google Scholar]
- 4. Ouchi Y, Rakugi H, Arai H, et al. Redefining the elderly as aged 75 years and older: proposal from the Joint Committee of Japan Gerontological Society and the Japan Geriatrics Society. Geriatr Gerontol Int 17: 1045-1047, 2017. [DOI] [PubMed] [Google Scholar]
- 5. Obana T, Fujita N, Noda Y, et al. Efficacy and safety of therapeutic ERCP for the elderly with choledocholithiasis: comparison with younger patients. Intern Med 49: 1935-1941, 2010. [DOI] [PubMed] [Google Scholar]
- 6. Ito Y, Tsujino T, Yamamoto O, et al. Endoscopic papillary balloon dilation for the management of bile duct stones in patients 85 years of age and older. Gastrointest Endosc 68: 477-482, 2008. [DOI] [PubMed] [Google Scholar]
- 7. Iida T, Kaneto H, Wagatsuma K, et al. Efficacy and safety of endoscopic procedures for common bile duct stones in patients aged 85 years or older: a retrospective study. PLoS One 13: e0190665, 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Kanamori A, Kiriyama S, Tanikawa M, et al. Long- and short-term outcomes of ERCP for bile duct stones in patients over 80 years old compared to younger patients: a propensity score analysis. Endosc Int Open 4: E83-E90, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Sugiyama M, Atomi Y. Endoscopic sphincterotomy for bile duct stones in patients 90 years of age and older. Gastrointest Endosc 52: 187-191, 2000. [DOI] [PubMed] [Google Scholar]
- 10. Katsinelos P, Paroutogou G, Kountouras J, Zavos C, Beltsis A, Tzovaras G. Efficacy and safety of therapeutic ERCP in patients 90 years of age and older. Gastrointest Endosc 63: 417-423, 2006. [DOI] [PubMed] [Google Scholar]
- 11. ASGE Training Committee, Jorgensen J, Kubiliun N, Law JK, et al. Endoscopic retrograde cholangiopancreatography (ERCP): core curriculum. Gastrointest Endosc 83: 279-289, 2016. [DOI] [PubMed] [Google Scholar]
- 12. Kiriyama S, Kozaka K, Takada T, et al. Tokyo Guidelines 2018: diagnostic criteria and severity grading of acute cholangitis (with videos). J Hepatobiliary Pancreat Sci 25: 17-30, 2018. [DOI] [PubMed] [Google Scholar]
- 13. Cotton PB, Eisen GM, Aabakken L, et al. A lexicon for endoscopic adverse events: report of an ASGE workshop. Gastrointest Endosc 71: 446-454, 2010. [DOI] [PubMed] [Google Scholar]
- 14. Ersoz G, Tekesin O, Ozutemiz AO, Gunsar F. Biliary sphincterotomy plus dilation with a large balloon for bile duct stones that are difficult to extract. Gastrointest Endosc 57: 156-159, 2003. [DOI] [PubMed] [Google Scholar]
- 15. Maydeo A, Bhandari S. Balloon sphincteroplasty for removing difficult bile duct stones. Endoscopy 39: 958-961, 2007. [DOI] [PubMed] [Google Scholar]
- 16. Minami A, Hirose S, Nomoto T, Hayakawa S. Small sphincterotomy combined with papillary dilation with large balloon permits retrieval of large stones without mechanical lithotripsy. World J Gastroenterol 13: 2179-2182, 2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Horiuchi A, Nakayama Y, Kajiyama M, et al. Biliary stenting in the management of large or multiple common bile duct stones. Gastrointest Endosc 71: 1200-1203, 2010. [DOI] [PubMed] [Google Scholar]
- 18. Li KW, Zhang XW, Ding J, Chen T, Wang J, Shi WJ. A prospective study of the efficacy of endoscopic biliary stenting on common bile duct stones. J Dig Dis. 10: 328-331, 2009. [DOI] [PubMed] [Google Scholar]
- 19. Ang TL, Fock KM, Teo EK, Chua TS, Tan J. An audit of the outcome of long-term biliary stenting in the treatment of common bile duct stones in a general hospital. J Gastroenterol. 41: 765-771, 2006. [DOI] [PubMed] [Google Scholar]
- 20. Sharma VK, Nguyen DD, Crowell MD, Lieberman DA, de Garmo P, Fleischer DE. A national study of cardiopulmonary un-planned events after GI endoscopy. Gastrointest Endosc 66: 27-33, 2007. [DOI] [PubMed] [Google Scholar]
- 21. Takahashi K, Tsuyuguchi T, Sugiyama H, et al. Risk factors of adverse events in endoscopic retrograde cholangiopancreatography for patients aged ≥85 years. Geriatr Gerontol Int 18: 1038-1045, 2018. [DOI] [PubMed] [Google Scholar]
- 22. Nishikawa T, Tsuyuguchi T, Sakai Y, et al. Old age is associated with increased severity of complications in endoscopic biliary stone removal. Dig Endosc 26: 569-576, 2014. [DOI] [PubMed] [Google Scholar]


