Abstract
The more than one million COVID-19 deaths in the United States include parents, grandparents, and other caregivers for children. These losses can disrupt the social, emotional, and economic well-being of children, their families, and their communities, and understanding the number and characteristics of affected children is a critical step in responding. We estimate the number of children who lost a parent or other co-residing caregiver to COVID-19 in the U.S. and identify racial, ethnic, and geographic disparities by aligning COVID-19 death counts through mid-May 2022 with household information from a representative sample of individuals. We estimate that 216,617 children lost a co-residing caregiver to COVID-19; 77,283 lost a parent and more than 17,000 children lost the only caregiver with whom they lived. Non-White children were more than twice as likely as White children to experience caregiver loss, and children under 14 years old experienced 70% of caregiver loss. These losses are a salient threat to the functioning of families and the communities in which COVID-19 deaths are concentrated, compounding additional challenges to physical and mental health and economic stability disproportionately imposed by the pandemic on historically disadvantaged populations. Policymakers and systems should take steps to ensure access to appropriate supports.
Keywords: COVID-19, Parental loss, Caregiver loss, Socioeconomic disparities, Child well-being
Introduction
The deaths of more than one million Americans to COVID-19 through mid-May 2022 threaten the functioning of family and social networks [4]. Among these deaths are parents, custodial grandparents, or others on whom children and youth relied [14], [19], and their sudden loss has ramifications for the children, the entire household, and their community as a whole.
The loss of a parent or other caregiver is likely to be a transformative moment in a child’s life [16]. Though most who experience parental loss manifest resilience, 5 to 10 percent demonstrate problems that include higher rates of mental health diagnoses like depression and anxiety [1], [18]; [30], higher rates of alcohol and substance abuse disorders[12], worse peer relationships [2], higher rates of suicide, and lower levels of educational attainment, adult employment, and other indicators of human capital [2], [10]; [20]; [22]. Though no research has documented the impacts of caregiver loss during the COVID-19 pandemic, the overall decline in youth mental health and disruptions in systems that would normally be available to bereaved youth likely increase the risk of negative outcomes among youth losing a parent since March 2020.
The risk for poor outcomes for children who lost a parent or caregiver to COVID-19 is compounded by the concentration of COVID-19 deaths in disadvantaged communities. Non-White populations have higher COVID-19 death rates than their White counterparts, with disparities concentrated among adults under age 65 [4]. Low-income individuals are at highest risk of death from COVID-19 and low-income counties faced disproportionately large shares of COVID-19 deaths, even after controlling for other indicators of well-being in two studies focused on individual and community-level associations with COVID-19 mortality rates of all persons [11, 28]. In addition, Black and Hispanic workers in low-wage, often consumer-facing, positions, have notably high rates of COVID-19 mortality [6]. These populations also have relatively high rates of health conditions associated with COVID-19 mortality, including overweight, obesity, diabetes, hypertension, and other morbidities [26, 33]. Thus, estimating the number and needs of children who lost a caregiver due to COVID-19 is a high priority for practitioners and policymakers interested in promoting resilience among these acutely vulnerable children and youth.
Prior efforts have sought to estimate parental or grandparent loss attributable to COVID-19. Kidman and colleagues estimated that 40,000 children lost a parent to COVID-19 through February, 2021, accounting for a 17–20% increase in parental loss relative to a period without COVID-19 [19]. A second team produced two reports. The first, as part of an assessment of global orphanhood attributable to COVID-19, estimated 137,000 children in the U.S. had lost at least one primary or secondary caregiver to COVID-19 through April 2021 [14, 15]. In a follow-up analysis, they estimated that 143,000 children had lost a biological parent or caregiving grandparent due to COVID-19 through June of 2021 [14]. While the latter studies acknowledge non-parental caregivers, both efforts rely heavily on biological parenthood, with limited consideration given to alternate family and household structures.
Changes in the structure of American households necessitate that we consider caregivers beyond biological parents in understanding the demographics and needs of bereaved children. Twenty-six percent of children and adolescents under 18, disproportionately low-income and Black or Hispanic, live with only a single caregiver [24]. In addition, 24% of children between birth and four years old, live in a multigenerational household; these children are, similarly, disproportionately non-White [25]. Many others live with a grandparent serving as a primary caregiver, whose deaths can have similar consequences as parental loss for a child [23]. Finally, a substantial proportion of children—disproportionately low-income, low-education, and Black or Hispanic—live in “doubled up” arrangements with non-family members, who may assume some caregiving role [9].
Merging COVID-19 death data with a representative survey of U.S. households, we estimate the counts and rates of COVID-19-related loss of any co-residing caregiver, allowing us to reflect current living situations. The resulting estimates are child-centric measures of caregiver loss based on demographic and geographic data for caregivers and children at the individual level.
Method
Data
We use data from two sources to compute the number of children who lost a parent or other co-residing caregiver to COVID-19. We obtained data on COVID-19 deaths through May 9, 2022, from the National Center for Health Statistics (NCHS), which provides data disaggregated by state, race and ethnicity, and age band. Estimates of caregiver loss also rely on population data from the U.S. Census Bureau’s American Community Survey Public Use Microdata Sample (PUMS) for the survey year 2019 (U.S. [32]. PUMS includes individual and household level data for more than 3 million individuals living in the United States, representing the demographic and household characteristics of the entire U.S. population. We used the PUMS dataset to compute the number of households, including the number of children younger than 18 years old living in each household and their relationship to each adult in that household. We considered all adults living in a household with a child to be a caregiver, and any parent to be a primary caregiver. Grandparents or adults were primary caregivers only when a parent was not present.
Analysis
We calculate COVID-19 death rates by dividing the number of COVID-19 deaths by age group, race/ethnicity, and state by the corresponding estimated size of that population segment (i.e., the weighted sample) from PUMS. We exclude people living in institutional and non-institutional group settings (like prisons or student dormitories) because they were unlikely to be actively living in households with children.
Children are any individual less than 18 years old. For households with at least one child, we first calculate a total household probability of death by summing the death rates of all adults. We subtract the death rate of the child, as the death of the child precludes the child from caregiver loss, as well as the probability of multiple caregiver deaths. We then multiply the probability of losing caregiver(s) in the households of children of each state, race/ethnicity, and age group by the corresponding weighted sample size, resulting in an estimate of the number of COVID-19 bereaved children. This allows us to calculate demographic characteristics associated with caregiver loss in relation to the children.
Results
We estimate that 216,617 U.S. children experienced the death of a caregiver with whom they lived, due to COVID-19 infection, between January 1, 2020, and May 9, 2022. This corresponds to about 1 out of every 336 children under the age of 18. Table 1 presents caregiver loss totals and rates by child’s age, race, ethnicity, and their relationship with the deceased caregiver. In fifty percent of cases (108,353), the child lost a primary caregiver to COVID-19; forty-five percent of cases (97,738) lost a parent, and an additional five percent (10,615) lost another primary caregiver, usually a grandparent. Nearly 85,000 (84,917) lost a grandparent, most frequently a grandparent in a multigenerational household that also included a parent. More than 17,000 children (17,042) lost their only co-residing caregiver.
Table 1.
Number and characteristics of children who lost a caregiver to COVID-19
| Number of children losing a co-residing caregiver | Rate of children losing a co-residing caregiver (Per 100,000) | |||
|---|---|---|---|---|
| Estimate | 95% confidence interval | Estimate | 95% confidence interval | |
| Total | 216,617 | (191,877, 241,357) | 298 | (264, 332) |
| By caregiver role | ||||
| Grandparent | 84,917 | (52,722, 117,111) | 117 | (72, 161) |
| Parent | 97,738 | (87,643, 107,833) | 134 | (121, 148) |
| Primary caregiver | 108,353 | (98,042, 118,664) | 149 | (135, 163) |
| Sole caregiver | 17,042 | (14,612, 19,473) | 23 | (20, 27) |
| By child race and ethnicity | ||||
| Hispanic | 78,217 | (69,939, 86,495) | 427 | (382, 472) |
| American Indian or Alaskan native | 5,224 | (3,517, 6,930) | 710 | (478, 942) |
| Non-Hispanic asian | 9,849 | (7,466, 12,232) | 281 | (213, 394) |
| Non-Hispanic black | 40,437 | (35,987, 44,886) | 418 | (372, 464) |
| Native Hawaiian or Pacific islander | 1,017 | (536, 1,498) | 679 | (358, 999) |
| Non-Hispanic white | 72,996 | (67,247, 78,745) | 200 | (185, 216) |
| Other or multiracial | 8,878 | (7,185, 10,571) | 226 | (183, 270) |
| By Child Age | ||||
| 0–4 | 43,977 | (37,372, 50,581) | 228 | (194, 262) |
| 5–13 | 108,641 | (96,631, 120,652) | 295 | (262,327) |
| 14–17 | 63,999 | (57,874, 70,124) | 386 | (349, 423) |
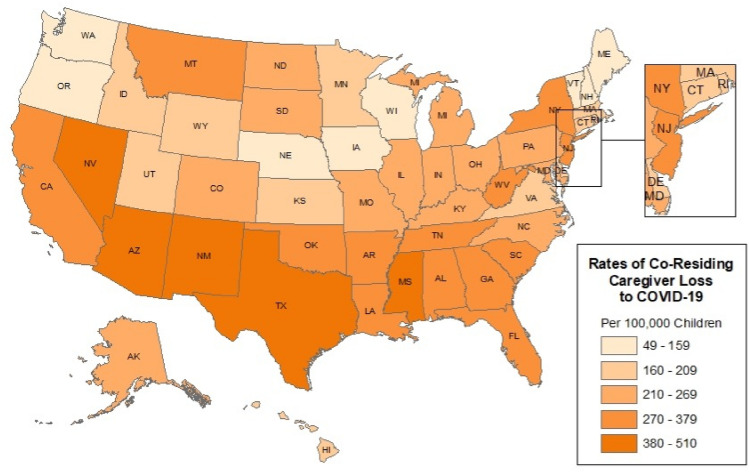
Caregiver loss occurs in every state, though counts and rates vary widely as shown in Fig. 1. California (32,843) and Texas (30,861) have by far the largest number of children who lost a caregiver, each more than double the caregiver loss counts in the next highest state of New York. Six states—California, Texas, New York, Florida, Arizona, and Georgia—account for half of national caregiver loss. There is less notable clustering when examining per capita rates of caregiver loss. New Mexico has the highest rate of caregiver loss (510 per 100,000), with four other states plus Washington, DC, also having caregiver loss rates exceeding 400 per 100,000. Vermont and New Hampshire have the lowest rates of caregiver loss while Vermont and Wyoming have the lowest counts.
Fig. 1.
Rates of co-residing caregiver loss to COVID-19 per 100,000 children
COVID-19 caregiver loss occurred in every racial and ethnic group considered, though losses are concentrated among non-White households. Children from non-White racial and/or Hispanic ethnic groups make up 66.3% of those who have lost a caregiver but only 50% of children in the U.S. population. Native Hawaiian/Pacific Islander children (HPI; 679 per 100,000) and American Indian or Alaskan Native children (AIAN; 710 per 100,000) had the highest per capita rates of caregiver loss; rates 3.4 and 3.55 times, respectively, higher than the rates of caregiver loss among White children. Hispanic and Non-Hispanic Black children had rates of caregiver loss 2.1 times those of White children. Hispanic children (78,217) accounted for the largest cohort of children that lost a caregiver to COVID-19. Notably, racial and ethnic disparities in caregiver loss exceed disparities in overall COVID-19 deaths [5].
Twenty percent of children experiencing caregiver loss (43,977) were from birth through 4 years old; 50.2% (108,641) were primary school age, from 5 through 13 years old, and the remaining 29.5% were 14 through 17 years old. Risk of losing a caregiver increased with the child’s age, ranging from 228 per 100,000 birth through 4 year old children to 386 per 100,000 children 14 through 17 years old. Disparities based on race and ethnicity were starkest for the youngest cohorts, as seen in Table 2. AIAN and HPI children under 5 years old had caregiver loss rates of 4.6 and 4.96 times their White peers, respectively, compared to 2.9 (AIAN and HPI) for their 14 through 17-year-old counterparts; similar age-based disparities were apparent for Hispanic, Non-Hispanic Black, and Non-Hispanic Asian children, though the differences by age were notably smaller.
Table 2.
COVID-19 Caregiver Loss by Race, Ethnicity, and Age: Estimates, Rates, and 95% Confidence Intervals
| Non-Hispanic Asian | Non-Hispanic Black | Native Hawaiian or Pacific Islander | Hispanic | American Indian or Alaskan Native | Non-Hispanic white | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| # | Rate Per 100,000 | # | Rate Per 100,000 | # | Rate Per 100,000 | # | Rate Per 100,000 | # | Rate Per 100,000 | # | Rate Per 100,000 | |
| 0–4 | 1,881 | 213 | 8,508 | 342 | 280 | 675 | 17,154 | 348 | 1,112 | 629 | 13,055 | 136 |
| (1,254, 2,508) | (142, 283) | (7,143, 9,872 | (287, 397) | (112, 448) | (269, 1080) | (14,996, 19,312) | (304, 392) | (626, 1,599) | (354, 905) | (11,693, 14,417) | (122, 150) | |
| 5–13 | 5,078 | 285 | 20,378 | 408 | 475 | 629 | 39,343 | 420 | 2,704 | 708 | 36,099 | 198 |
| (3,857, 6,298) | (216, 353) | (18,349, 22,407) | (367, 449) | (271, 679) | (359, 898) | (35,337, 43,350) | (377, 463) | (1,861, 3,547) | (488, 929) | (33,274, 38,924) | (182, 213) | |
| 14–17 | 2,891 | 347 | 11,551 | 527 | 262 | 798 | 21,720 | 540 | 1,407 | 796 | 23,841 | 278 |
| (2,355, 3,426) | (283, 412) | (10,494) | (479, 576) | (153, 371) | (457, 1,130) | (19,606, 23,834) | (487, 593) | (1,030, 1,784) | (583, 1,009) | (22,279, 25,404) | (260, 297) | |
Disparities in caregiver loss by the decedent’s relationship to child largely follow overall trends, though there are some noteworthy distinctions. Black (65 per 100,000) and AIAN (64 per 100,000) children were most likely to lose their only co-residing caregiver. Asian children had the lowest rate of parental or any primary caregiver loss and their rate of losing their sole co-residing caregiver was 39% that of White children, the next lowest category.
Discussion
An estimated 216,617 children lost a co-residing caregiver who died of COVID-19 in the U.S. as of May 9, 2022. This is about 1 out of every 336 Americans under 18 years old. Many (97,738) lost their parent, nearly 85,000 children experienced the death of a grandparent caregiver, and at least 33,962 lost another adult with whom they lived. More than 17,000 children lost their only co-residing caregiver and are thus especially vulnerable. The current findings are largely consistent with past efforts to estimate the number of caregivers who have died of COVID-19 [14]; [19]. We updated those estimates and expanded on them by using data from the PUMS, which allowed us to assess loss in relation to detailed child demographics including current household structure, age, race, ethnicity, and state of residence.
Children and families who experience loss must adapt to life without the caregiver; this will include coping with grief and, for many, renegotiating family roles, responsibilities, and meeting basic physical, material, emotional, and cognitive needs. Although, most children who lose a caregiver will demonstrate resilience and healthy development, others will struggle with grief complicated by traumatic stress, other symptoms, or other developmental problems [17]. The context of the COVID-19 pandemic presents additional challenges because important resources to promote positive adaptation and financial stability may be more difficult to access due to remote education, social-distancing that impacts supportive relationships, or strained mental health, health, and social services. That COVID-19 deaths occur disproportionately among vulnerable communities exacerbates the challenge of accessing services for many bereaved children.
A comprehensive response to caregiver loss will include resources to promote resilience for children, youth, and families who need different levels of support. Providing the necessary range of supports for more than 200,000 children and their families requires coordinated efforts from health and mental health systems, community-based organizations, philanthropies, and federal, state, and local policymakers whose attention and funding are critical to the success of a comprehensive, substantive, and sustained effort. They should leverage existing infrastructures like schools and pediatric health care settings that routinely interact with children, screen for social needs, and are putative service hubs. Early childhood education facilities, faith-based institutions, youth sports leagues, and other community-based settings in which adults routinely interface with children and youth provide additional opportunities to identify and serve bereaved children.
A coordinated response to caregiver loss must target resources to the vulnerable communities bearing the disproportionate share of COVID-19 deaths. Caregiver death was concentrated in the most populous states (e.g., California, Florida, Georgia, New York, and Texas), among older children, and among racial and ethnic groups that have been systemically marginalized in the U.S. Non-White and/or Hispanic children constituted two-thirds of caregiver loss, with caregiver loss rates more than double those of White, non-Hispanic children. Disparities of caregiver loss by race and ethnicity exceed disparities in COVID-19 deaths; this is likely due to both the higher COVID-19 death rate among Non-White adults under 65 and the higher average number of adult caretakers among children identified as Hispanic, American Indian and Alaskan Native, and Native Hawaiian or Other Pacific Islander, compared to their Non-Hispanic White counterparts. Our ability to observe more specific geographic and demographic disparities is constrained by the limitations of available data, but we can infer from other analyses that caregiver loss is even more heavily concentrated in vulnerable populations than shown in our results. Findings from Seligman, Ferranna, and Bloom [28], Chen and colleagues [6], and Gross and colleagues [11] suggest that these losses are concentrated among low-income households and in lower-income communities that have been the subject of systemic disinvestment that may deprive children of resources critical for adapting to adversity. Such disadvantage usually spans generations and can cumulatively constrain the development of individual resources (e.g., educational attainment,emotional and behavioral regulation skills) and opportunities for external support (family functioning and other close relationships; effective health and human services) that are central to promoting and protecting positive outcomes [13].
The infrastructure to support affected households, especially in marginalized communities in which COVID-19 deaths are concentrated, must be buttressed through investments in capacity and grief competence. Professionals who interact with grieving children in normative settings like classrooms, community-based nonprofits, and primary care providers, are often poorly prepared to address their needs, and low-cost and free capacity building programs available to organizations already embedded within vulnerable communities may efficiently fill that gap for children whose needs are limited to preventative grief services [21]. For children whose needs include more clinical services like psychotherapy, mental health care—of which there is a national shortage—may be unavailable or unaffordable for communities hit hardest by COVID-19, and clinicians often lack training in grief-focused therapies [7, 27]. Grief-focused training programs may allow existing providers to offer appropriate care. Policymakers, health systems, and insurance providers can also explore options to expand access to mental health care where it is unavailable or unaffordable through new telehealth options and reductions in patients’ cost-sharing responsibilities for grief-focused care. In the long-term, mental health professional training programs may seek to increase training in grief-focused care as well as recruitment among rural, low-income, and non-White populations who may be more likely and more able to provide culturally competent care in underserved communities.
Families in particularly vulnerable communities will also disproportionately need financial support to weather the costs a caregiver’s death and potential lost income; these challenges are especially salient given that COVID-19 deaths among working-age adults disproportionately include low-wage workers unlikely to have sufficient savings or life insurance policies to sustain their households for an extended period. Health and social service entities that interface with bereaved families should identify those that may be eligible for existing mechanisms of financial support, like Social Security Survivor’s Benefits, the Federal Emergency Management Agency’s Funeral Reimbursement Program, the Child Tax Credit, and means-tested programs like Temporary Assistance for Needy Families, the Supplemental Nutrition Assistance Program and Medicaid. In addition, there is precedent for ad hoc efforts from the public and philanthropic sectors to provide interim and supplementary financial assistance to victims of disasters [8, 29].
Limitations
This study has limitations. First, estimates based on extrapolation are subject to inherent uncertainty, which we sought to minimize. Second, COVID-19 deaths among some racial and ethnic groups—people of Hispanic ethnicity or those identifying their race as American Indian or Alaska Native, Asian or Pacific Islander—may have been undercounted; thus, our estimates of their caregiver loss should be interpreted as lower bounds [3]. Third, we rely on 2019 population data, as pandemic-related complications rendered 2020 population estimates from the American Community Survey “experimental” [31]. More recent data may better reflect the distributions of demographic factors and COVID-19 deaths.
Conclusions
Many children in the U.S. have lost a caregiver to COVID-19. Most lost a parent, including a sizeable number of children who lost their only caregiver. Caregiver deaths are ubiquitous, spanning the entire country and all demographic categories, though they are concentrated among children and youth from marginalized racial and ethnic groups. These children and their families must confront the processes of grief while also meeting developmental needs required for long-term positive outcomes. Restrictions and other consequences of the COVID-19 pandemic present special challenges as children, families, and communities attempt to promote resilience. A comprehensive response to this phenomenon must be adaptable to the varying needs of children while targeting the vulnerable communities that faced the largest share of COVID-19 deaths with the fewest resources with which to cope.
Author Contributions
DT: guided the conceptualization, data analysis, and writing, wrote sections of the first draft of the manuscript, prepared tables, and critically reviewed and contributed to the full manuscript; JJC: contributed to the conceptualization of the manuscript, wrote sections of the first draft of the manuscript, and critically reviewed and contributed to the full manuscript; KA: conducted statistical analyses, verified the underlying data, wrote the first draft of the methods section, and critically reviewed and contributed to the full manuscript; JB: contributed to the conceptualization of the study and critically reviewed and contributed to the full manuscript.
Funding
Funding was provided through the COVID Collaborative from the Allstate Foundation, the Helmsley Charitable Trust, New York Life Foundation, the Skoll Foundation, and the Walton Family Foundation.
Data Availability
Data are from publicly available sources, though a compiled dataset has not been made publicly available. Interested parties can contact the corresponding author to access the data included in this analysis.
Code Availability
Interested parties may contact the corresponding author to obtain the code used to produce results included in this manuscript.
Declarations
Conflicts of interest
Mr. Bridgeland is CEO of the COVID Collaborative, a national assembly of experts, leaders and institutions in health, education and the economy and associations representing the diversity of the country to turn the tide on the pandemic by supporting global, federal, state, and local COVID-19 response efforts. Drs. Treglia, Cutuli, and Arasteh received funding for this study through the COVID Collaborative and Social Policy Analytics. Dr. Treglia is CEO of Social Policy Analytics and an Expert Contributor to the COVID Collaborative, with whom he consults on COVID-19 related caregiver loss.
Ethical Approval
This study was reviewed by the Nemours Children’s Health Institutional Review Board and deemed not to be human subjects research.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Footnotes
We have received expertise and general advice from many people whose collective contributions are critical to this work, and we thank them for their time, patience, and commitment to helping children suffering the loss of a parent or other caregiver. In particular, we want to thank Dr. Randall Kuhn for his methodological guidance, Dr. Bikki Tran Smith for creating the maps contained within our manuscript, and Delaney Michaelson for her general research and organizational efforts. We also wish to acknowledge funding from the Allstate Foundation, the Helmsley Charitable Trust, New York Life Foundation, the Skoll Foundation, and the Walton Family Foundation that made this work possible.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Berg L, Rostila M, Hjern A. Parental death during childhood and depression in young adults – a national cohort study. Journal of Child Psychology and Psychiatry and Allied Disciplines. 2016;57(9):1092–1098. doi: 10.1111/jcpp.12560. [DOI] [PubMed] [Google Scholar]
- 2.Brent DA, Melhem NM, Masten AS, Porta G, Payne MW. Longitudinal effects of parental bereavement on adolescent developmental competence. Journal of Clinical Child and Adolescent Psychology. 2012;41(6):778–791. doi: 10.1080/15374416.2012.717871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.CDC. (2021). Health Disparities Provisional Death Counts for Coronavirus Disease 2019 (COVID-19).
- 4.Centers for Disease Control and Prevention. (2021). Distribution of COVID-19 Deaths and Populations, by Jurisdiction, Age, and Race and Hispanic Origin. Retrieved December 22, 2021, from https://data.cdc.gov/NCHS/Distribution-of-COVID-19-Deaths-and-Populations-by/jwta-jxbg
- 5.Centers for Disease Control and Prevention. (2022). Risk for COVID-19 Infection, Hospitalization, and Death By Race/Ethnicity. Retrieved February 15, 2022, from https://www.cdc.gov/coronavirus/2019-ncov/covid-data/investigations-discovery/hospitalization-death-by-race-ethnicity.html
- 6.Chen YH, Glymour M, Riley A, Balmes J, Duchowny K, Harrison R, Bibbins-Domingo K. Excess mortality associated with the COVID-19 pandemic among Californians 18–65 years of age, by occupational sector and occupation: March through November 2020. PLoS ONE. 2021;16:1–10. doi: 10.1371/journal.pone.0252454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cicchetti RJ, McArthur L, Szirony GM, Blum C. Perceived competency in grief counseling: Implications for counselor education. Journal of Social, Behavioral, and Health Sciences. 2016;10(1):3–17. doi: 10.5590/jsbhs.2016.10.1.02. [DOI] [Google Scholar]
- 8.E4E Relief. (2021). Brave of Heart Fund. Retrieved July 2, 2022, from https://employeerelieffund.org/brave-of-heart-fund
- 9.Eggers FJ, Moumen F. Analysis of Trends in Household Composition Using American Housing Survey Data. SSRN Electronic Journal. 2014 doi: 10.2139/ssrn.2445476. [DOI] [Google Scholar]
- 10.Gimenez L, Chou S-Y, Liu J-T, Liu J-L. Parental loss and children ’ s well- being. Journal of Human Resources. 2013;48:1035–1071. doi: 10.1353/jhr.2013.0028. [DOI] [Google Scholar]
- 11.Gross CP, Essien UR, Pasha S, Gross JR, Wang SY, Nunez-Smith M. Racial and ethnic disparities in population-level Covid-19 mortality. Journal of General Internal Medicine. 2020;35(10):3097–3099. doi: 10.1007/s11606-020-06081-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hamdan S, Melhem NM, Porta G, Song MS, Brent DA. Alcohol and substance abuse in parentally bereaved youth. The Journal of Clinical Psychiatry. 2013 doi: 10.4088/JCP.13m08391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Herbers JE, Hayes KR, Cutuli JJ. Adaptive systems for student resilience in the context of COVID-19. School Psychology. 2021;36(5):422–426. doi: 10.1037/spq0000471. [DOI] [PubMed] [Google Scholar]
- 14.Hillis SD, Blenkinsop A, Villaveces A, Annor FB, Liburd L, Massetti GM, Unwin HJT. COVID-19-associated orphanhood and caregiver death in the United States. Pediatrics. 2021;148:e2021053760. doi: 10.1542/peds.2021-053760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hillis SD, Unwin HJT, Chen Y, Cluver L, Sherr L, Goldman PS, Flaxman S. Global minimum estimates of children affected by COVID-19-associated orphanhood and deaths of caregivers: A modelling study. The Lancet. 2021;398(10298):391–402. doi: 10.1016/S0140-6736(21)01253-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Joint United Nations Programme on HIV/AIDS. (2009). National AIDS Spending Assessment (NASA): Classification and definitions. Geneva: UNAIDS. Available from https://www.unaids.org/sites/default/files/media_asset/jc1557_nasa_en_0.pdf
- 17.Kaplow JB, Layne CM, Pynoos RS, Cohen JA, Lieberman A. DSM-V diagnostic criteria for Bereavement- Related Disorders in children and adolescents: Developmental considerations. Psychiatry. 2012;75(3):243–266. doi: 10.1521/psyc.2012.75.3.243. [DOI] [PubMed] [Google Scholar]
- 18.Keyes KM, Pratt C, Galea S, Mclaughlin KA, Koenen KC, Shear MK. The burden of loss: unexpected death of a loved one and psychiatric disorders across the life course in a national study. American Journal of Psychiatry. 2014;171:864–781. doi: 10.1176/appi.ajp.2014.13081132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kidman R, Margolis R, Smith-Greenaway E, Verdery AM. Estimates and projections of COVID-19 and parental death in the U.S. Journal of the American Medical Association. 2021;175(7):745–746. doi: 10.1111/cen.12738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Li J, Vestergaard M, Cnattingius S, Gissler M, Bech BH, Obel C. Mortality after parental death in childhood: a nationwide cohort study from three Nordic countries. National Library of Medicine. 2014;11:e1001679. doi: 10.1371/journal.pmed.1001679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.New York Life Foundation, & American Federation of Teachers. (2020). Grief in School survey: key findings and topline results.
- 22.Parsons, S. (2011). Long-term impact of childhood bereavement, 1–22.
- 23.Pew Research Center. (2013). Grandparents living with or serving as primary caregivers for their grandchildren.
- 24.Pew Research Center. (2015). Parenting in America: Outlook, worries, aspirations are strongly linked to financial situation. Numbers, Facts and Trends Shaping the World. Retrieved from https://www.pewresearch.org/social-trends/2015/12/17/parenting-in-america/
- 25.Pilkauskas NV, Amorim M, Dunifon RE. Historical trends in children living in multigenerational households in the United States: 1870–2018. Demography. 2020;57(6):2269–2296. doi: 10.1007/s13524-020-00920-5. [DOI] [PubMed] [Google Scholar]
- 26.Rosenstock S, Whitman S, West JF, Balkin M. Racial Disparities in Diabetes Mortality in the 50 Most Populous US Cities. Journal of Urban Health. 2014;91(5):873–885. doi: 10.1007/s11524-013-9861-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.SAMHSA. (2020). Double Jeopardy: COVID-19 and Behavioral Health Disparities for Black and Latino Communities in the U.S. Kaiser Family Foundation.
- 28.Seligman B, Ferranna M, Bloom DE. Social determinants of mortality from COVID-19: A simulation study using NHANES. PLoS Medicine. 2021;18(1):1–13. doi: 10.1371/journal.pmed.1003490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.September 11th Victims Compensation Fund. (2021). Annual Report 2020.
- 30.Simbi CMC, Zhang Y, Wang Z. Early parental loss in childhood and depression in adults: A systematic review and meta-analysis of case-controlled studies. Journal of Affective Disorders. 2020;260:272–280. doi: 10.1016/j.jad.2019.07.087. [DOI] [PubMed] [Google Scholar]
- 31.U.S. Census Bureau. (2021a). 2020 ACS 1-Year Public Use Microdata Sample with Experimental Weights. Retrieved February 10, 2022, from https://www.census.gov/programs-surveys/acs/data/experimental-data/2020-1-year-pums.html
- 32.U.S. Census Bureau. (2021b). Accessing PUMS Data. Retrieved October 10, 2021, from https://www.census.gov/programs-surveys/acs/microdata/access.2019.html
- 33.Zhang H, Rodriguez-Monguio R. Racial disparities in the risk of developing obesity-related diseases: A cross-sectional study. Ethnicity and Disease. 2012;22(3):308–316. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are from publicly available sources, though a compiled dataset has not been made publicly available. Interested parties can contact the corresponding author to access the data included in this analysis.
Interested parties may contact the corresponding author to obtain the code used to produce results included in this manuscript.